ESIL Reflections COVID-19 Series – States’ Resilience to Future Health Emergencies – Connecting the Dots between Core Obligations and Core Capacities
 PDF Version
PDF Version
Vol 9, Issue 2
Editorial board: Federico Casolari, Patrycja Grzebyk, Ellen Hey, Guy Sinclair and Ramses Wessel (editor-in-chief)
Brigit Toebes (University of Groningen)
Introduction
Covid-19 has put a spotlight on the responsibilities of States under the International Health Regulations and on State accountability in case of a breach.[1] In addition, there has been much debate about how measures to protect against Covid-19 infringe on the enjoyment of civil and political rights, in particular rights to privacy and freedom of movement.[2] It will be important to evaluate these matters carefully given the current crisis.
While these approaches and dimensions are valuable, we should also look beyond this crisis and address country preparedness to future infectious disease outbreaks. To this end, this Reflection assesses how according to international law, all countries around the world are required to be prepared to respond to a future public health emergency. It does so from the perspective of the right to health as an economic and social right, in interaction with the International Health Regulations (IHR). This contribution is grounded in the understanding that Covid-19 reflects, in essence, a crisis of the right to health: because countries do not deliver the right to health as reflected by the IHR, many other problems including violations of international law arise.
The right to health
To understand the interaction between the right to health and the IHR, one must go back to the period right after WWII. It was a period of optimism and belief in a better and healthier world, a time where the idea was voiced that ‘medicine is one of the pillars of peace’.[3] Already in 1946, the Constitution of the World Health Organization (WHO) was adopted, the founding document of the Organization, which led to WHO’s establishment in 1948. It is a remarkable and ground-breaking document in many ways. The Preamble to the WHO Constitution defines health as a ‘state of complete physical, mental and social well-being, and not merely the absence of disease’. This definition has often been criticized for being too absolute, yet it should be seen in the light of post-war idealism, and can be appreciated for its reference to mental and social well-being as important dimensions of health.[4]
The Preamble was also pioneering for its recognition of health as a right: ‘the enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition’. This wording informed the right to health provisions in the UN human rights treaties that were adopted in the decades thereafter. Probably, the most authoritative provision is Article 12 of the International Covenant on Economic, Social and Cultural Rights (ICESCR, 1966), which stipulates the ‘right to the highest attainable standard of health’. Other key provisions include Article 12 of the Convention on the Elimination of Discrimination Against Women (CEDAW, 1979), Article 24 of the Convention on the Rights of the Child (CRC, 1989), and Article 25 of the Convention on the Rights of Persons with Disabilities (CRPD, 2006). Early this century, Articles 12 ICESCR and 24 CRC have been complemented with General Comments, explanatory documents which carry the status of soft law but are nonetheless seen as authoritative.[5]
As indicated already, the WHO was the first international organization to recognize the right to health as a human right. However, over the past 73 years of its existence, the WHO has not manifested itself as a human rights organization. Yet the Organization has gradually embraced the human rights framework owing to the way that it has been developed by the UN human rights mechanisms.
The International Health Regulations
The WHO Constitution grants considerable legislative powers to the World Health Assembly (WHA). Based on Articles 19-23, the WHA may adopt conventions, (binding) regulations, and (non-binding) recommendations. The results have been very disappointing so far: since its establishment in 1948, the WHO has only adopted one treaty (the Framework Convention on Tobacco Control) and two regulations (the Nomenclature Regulations and the IHR). While the results are scant, the Framework Convention on Tobacco Control and the IHR are highly authoritative instruments. Central to this Reflection are of course the IHR.
International collaboration in the field of infectious disease control started in the second half of the 19th century. In 1851, the first international sanitary conference took place. Many similar meetings followed, and subsequent sets of international sanitary regulations were gradually adopted, instruments which precede the current IHR. Since its establishment in 1948, the WHO adopted Regulations in 1951 and 1969, and 2005 – currently the most recent set, which is binding since 2007. Given its status as Regulations, the IHR is binding on all 194 WHO Members without their consent (although Members may notify the Director-General of rejection or reservations).
The new IHR is innovative because of its ‘all hazards’-approach: risks arising from numerous sources are covered, not just a limited list of diseases.[6] Thus, even a terrorist attack with anthrax, or a chemical spill, could fall within the remit of this instrument if it is established that the threat constitutes a ‘public health emergency of international concern’ (PHEIC).[7] A PHEIC has occurred six times since the adoption of the revised IHR: influenza in Mexico (2009); Ebola in West Africa (2014); polio in Pakistan, Afghanistan and Nigeria (2014); Zika in South America (2016); Ebola in Congo (2018); and Covid-19 in China (2019).
The IHR refers to human rights in various provisions (Articles 3, 23, 32, and 45). These references are, in essence, linked to the respect for civil and political rights including rights to privacy, physical integrity and freedom of movement (e.g. medical consent in Article 23 and respect for travellers in Article 32). Contrary to the WHO Constitution and the Framework Convention on Tobacco Control, the IHR does not mention the right to health.[8] This is an important omission, given that – as I will demonstrate below – the State’s obligation to prepare and respond to infectious disease outbreaks is an essential component of the right to health.
Another important shortcoming of the IHR is its lack of sanctions: States refusing to collaborate with the WHO in case of an outbreak can go without any warning or punishment. As I will argue below, the UN human rights monitoring system may offer complementary mechanisms for holding States accountable.
Core obligations and core capacities: connecting the dots
My main point is that the core obligations under the right to health are closely intertwined with the core capacities under the IHR. Starting with the UN human rights framework, I will now briefly discuss both regimes and discuss their interaction with each other. The key provision stating the right to health is Article 12 ICESCR, which stipulates that States should take steps necessary for ‘(c) The prevention, treatment and control of epidemic, endemic, occupational and other diseases.’ Hence, there is a clear human rights obligation on the part of states to take measures to combat epidemic diseases. An explanation of the meaning and scope of the right to health is provided in General Comment 14 to Article 12 ICESCR. As a General Comment, this instrument is not legally binding, yet is seen as (highly) authoritative. Two recognized components from this General Comment are important for infectious disease control:
AAAQ – according to the General Comment, the right to health contains a set of interrelated and essential elements, which are considered to provide guidance to the actions by States: availability, accessibility, acceptability and quality. Accessibility has four overlapping dimensions (see Table I). This so-called ‘AAAQ’ is an authoritative set of standards that is increasingly applied across international and domestic health settings. While it certainly lacks precision, it helps to identify the weak spots in health decision making. Given that these (and similar) principles are applied frequently in health settings and because their importance is underscored by governments and health authorities, I suggest that this framework is emerging as a norm of customary international (health) law.
The AAAQ is also very informative in the context of Covid-19, as it pinpoints the weak spots in this crisis. Firstly, key problems in this crisis relate to a lack of availability of health personnel, intensive care beds and drugs, masks and gloves. Furthermore, many problems occur in the context of accessibility, e.g. discrimination in access to healthcare of vulnerable persons (older persons, persons with low socio-economic status, persons with underlying health conditions), and a lack of geographically accessible, affordable and good quality healthcare. Thirdly, in terms of acceptability, Covid-19 creates many complex healthcare settings where medical ethics are under threat, for example in care homes where older and disabled persons are denied any contact with the outside world. Lastly, in terms of quality, due to a scarcity of properly trained personnel and suitable medical equipment, many are deprived from accessing good quality healthcare. Again, while this framework lacks precision and may not be used to identify concrete human rights violations, it helps to frame the analysis and debate about how the right to health is guaranteed in the context of Covid-19, and it shows to what extent countries are prepared to address the next crisis.
Core obligations – the second concept in the right to health framework that is of key importance to infectious disease control is the recognition of ‘core obligations’ under the right to health. General Comment No. 14 on Article 12 ICESCR refers to General Comment No. 3, in which the Committee on Economic, Social and Cultural Rights (CESCR) confirms that States parties have ‘a core obligation to ensure the satisfaction of, at the very least, minimum essential levels of each of the rights enunciated in the Covenant, including essential primary health care’. The meaning of this concept has been discussed extensively in human rights discourse, and interpretations regarding its scope differ.[9] Importantly, there is confusion as to whether the core obligations in the right to health are non-derogable (cannot be limited in any way), or whether resource scarcity may be an excuse for Governments not to deliver the core.[10] But the idea of a core content – and the notion that there is a basic subsistence line below which no government should fall – is informative in a crisis setting, where resources are limited.
For the identification of the specific core obligations under the right to health, General Comment 14 makes reference to the Programme of Action of the International Conference on Population and Development (1994)[11] and WHO’s Alma-Ata Declaration (1978),[12] stating that these programmes provide ‘compelling guidance’ on the core obligations arising from Article 12. The Committee identifies a set of core obligations, four of which are particularly relevant to the Covid-19 crisis (Table I).
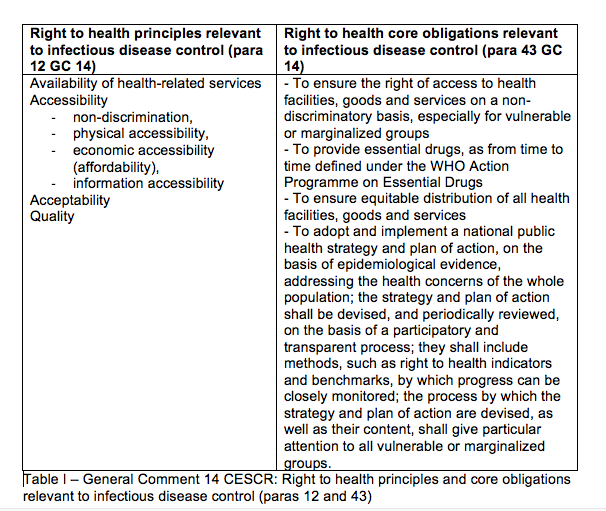
In essence, all the principles and obligations set out in Table I are related to the duty of States to build resilient health systems.
Core capacities – alongside the core content of the right to health outlined above, there are the core capacities under the IHR, which are aimed at preparing States to respond adequately to a public health emergency. IHR’s core capacities are identified under Articles 5, 13, Annex I, and in a considerable amount of subsequent technical documentation. Importantly, Article 13 requires States parties to develop within five years ‘the capacity to respond promptly and effectively to public health risks and public health emergencies of international concern’. The parallels with the core obligations under the right to health are striking: as set out in Table I, the right to health framework requires States to ‘adopt a national public health strategy and plan of action, on the basis of epidemiological evidence (…)’.
A closer look at the definition of core capacities under the IHR helps to understand the nature of this undertaking, and gives more substance to the not so detailed wording under the right to health. The IHR core capacities should enable States Parties to meet the key objectives of the IHR as set out in Article 2: ‘to prevent, protect against, control and provide a public health response to the international spread of disease (…).’ Gostin and Katz explain that core capacities are required at national, regional and local levels to detect unexpected mortality, report essential information, confirm and assess the status of reported events, notify the WHO, and respond effectively to contain and mitigate the event.[13] The IHR monitoring process involves assessment of the development and implementation of eight core capacities at points of entry and for IHR-related hazards (See Table II).[14]
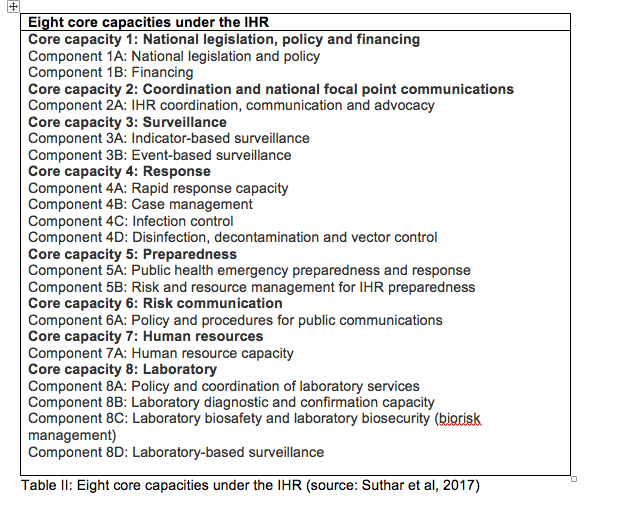
From a legal perspective, the first core capacity is of key importance. According to the WHO, States Parties need to have an ‘adequate legal framework to support and enable implementation of all of their obligations and rights. In some States Parties, implementation of the IHR may require that they adopt implementing or enabling legislation for some or all of these obligations and rights.’ Furthermore, ‘even where new or revised legislation may not be specifically required under the State Party’s legal system for implementation of provisions in the IHR (2005), States may still choose to revise some legislation, regulations or other instruments in order to facilitate implementation in a more efficient, effective or beneficial manner.’[15] After Covid-19, many States will have to evaluate and, where necessary, revise their domestic legislation in the field of infectious disease control.
While these efforts to build core capacities are worthwhile, evidence suggests that the implementation and monitoring of the core capacities remains a challenge. Suthar et al report that in 2014, only 64 States Parties reported meeting core capacities.[16] According to Gostin and Katz, many countries lack the financial resources to meet the core capacities, while high income countries have offered little financial support.[17] Suthar et al also suggest that there is limited knowledge on how countries should achieve the core capacities domestically. Initially, the whole process was only subject to self-evaluation. At the sixty-eighth World Health Assembly in 2015, the idea of voluntary external evaluations was introduced.[18] One of the existing evaluations is the (US-funded) Joint External Evaluation (JEE), a voluntary process to assess country capacities to prevent, detect and respond to public health risks. Thus far, around 100 countries have been evaluated through this process.[19] In detailed reports, the strengths and weaknesses of countries under scrutiny are analysed. While these processes are worthwhile and may strengthen the implementation and enforcement of the IHR, overall enforcement of the IHR remains weak.
Conclusions
There are considerable parallels between States’ obligations to have core capacities under the IHR, and their ‘minimum core obligations’ under the human right to health. I argue in favour of more cross-fertilisation between both regimes. This regime-interaction may enrich both frameworks from a normative perspective while it may also enhance accountability. In particular, normative interaction may arise through a systemic interpretation of the IHR, as based on Article 31(3)(c) of the Vienna Convention on the Law of Treaties (VCLT), which provides that ‘international standards may be interpreted in the light of any relevant rules of international law applicable in the relations between the parties’. The comprehensive IHR framework gives more detail to the open-ended wording under the right to health framework. Subsequently, the recognition that the IHR core capacities might inform the content of the human right to health, suggests that if States fail to comply with the IHR, they may be held accountable under the UN human rights regime, e.g. the reporting procedures and individual complaint mechanisms of the CESCR, CRC, CEDAW and CRPD, as well as the UN Special Procedures.
More generally, there is an urgent need to perceive public health emergencies as a matter of international human rights obligation and accountability. The right to health entails that Governments should evaluate their preparedness for the next global public health emergency, whether it comes from within their own borders or from abroad. Governments should do so in close consultation with WHO, the most authoritative organization globally when it comes to infectious disease outbreaks, which has generated a wealth of expertise over the course of its existence. And because the WHO is unable to sanction, the ultimate consequence when States fail to comply with their obligations should be accountability under the UN human rights regime.
Cite as: Brigit Toebes, ‘States’ Resilience to Future Health Emergencies: Connecting the Dots between Core Obligations and Core Capacities, ESIL Reflections 9:2 (2020).
*Prof Brigit Toebes holds the Chair of Health Law in a Global Context at the Faculty of Law of the University of Groningen in the Netherlands. For this post, she wishes to thank her student Anna Gedevanishvili for her inspiration and advice.
[1] E.g. Pedro Villareal, ‘The (not so) Hard Side of the IHR: Breaches of Legal Obligations’, Global Health Law Groningen Blog, 26 February 2020, available at https://www.rug.nl/rechten/onderzoek/expertisecentra/ghlg/blog/the-not-so-hard-side-of-the-ihr-breaches-of-legal-obligations-26-02-2020 (accessed 28 May 2020).
[2] E.g. Antoine Buyse and Roel de Lange, The Netherlands: of Rollercoasters and Elephants, Verfassungsblog, 8 May 2020, available at https://verfassungsblog.de/author/antoine-buyse/ (accessed 28 May 2020).
[3] Statement by Archbishop Spellman in a Memorandum presented at the United Nations Conference on International Organization held in San Francisco in 1945. See Toebes, 1999.
[4] For a discussion see Brigit Toebes, The Right to Health as a Human Right in International Law, Antwerp/Groningen/Oxford: Intersentia-Hart: 1999, pp. 28-36.
[5] UN Committee on Economic, Social and Cultural Rights (CESCR), The Right to the Highest Attainable Standard of Health, UN General Comment No 14 (2000), UN Doc E/C12/200/4, 11 August 2000; CESCR, General Comment 15 (2013) on the rights of the child to the enjoyment of the highest attainable standard of health (art 24), UN Doc. CRC/C/GC/15, 17 April 2013.
[6] Lawrence O. Gostin, ‘The International Health Regulations: Responding to Public Health Emergencies of International Concern’, in Lawrence O. Gostin, Global Health Law, Harvard University Press, 2014, pp. 177-204, at p. 185.
[7] See also Stefania Negri, ‘Communicable disease control’, in Gian Luca Burci and Brigit Toebes, Research Handbook on Global Health Law, Cheltenham/Northampton: Edward Elgar Publishing, 2018.
[8] With the exception of a reference to right to health information in Article 45.
[9] See also Lisa Forman et al, ‘What could a strengthened right to health bring to the post-2015 health development agenda? Interrogating the role of the minimum core concept in advancing essential global health needs’, BMC International Health and Human Rights, 13 (48) 2013.
[10] For this, compare the language of General Comments 3 and 14 CESCR and 15 CRC. See also Lisa Forman et al, 2013.
[11] UNFPA Programme of Action of the International Conference on Population and Development, adopted in Cairo, 5-13 September 1994 available at https://www.unfpa.org/sites/default/files/event-pdf/PoA_en.pdf (accessed 7 June 2020).
[12] WHO, International Conference on Primary Health Cara, Alma Ata, USSR, 6-12 September 1978, available at https://www.who.int/publications/almaata_declaration_en.pdf?ua=1 (accessed 7 June 2020).
[13] For a detailed analysis see Lawrence O. Gostin and Renecca Katz, ‘The International Health Regulations: The Governing Framework for Global Health Security’, The Milbank Quarterly, 2016 June; 94(2): 264–313.
[14] See IHR questionnaire, available at https://apps.who.int/iris/bitstream/handle/10665/255756/WHO-WHE-CPI-2017.41-eng.pdf;jsessionid=B84A8C50E5ECA19649F4DCE13E8AE608?sequence=1 (accessed 30 May 2020). For an analysis see Amitabh B. Sutahr et al, ‘Lessons learnt from implementation of the International Health Regulations: a systematic review’, Bulletin of the World Health Organization 2018;96:110-121E. Available at https://www.who.int/bulletin/volumes/96/2/16-189100/en/ (accessed 30 May 2020).
[15] WHO, strengthening health security by Implementing the International Health Regulations, at https://www.who.int/ihr/legislation_policy/en/ (accessed 30 May 2020). ‘Obligations and rights’ refers to rights and obligations of States, not of individuals.
[16] WHO, Implementation of the International Health Regulations (2005): report of the Review Committee on Second Extensions for Establishing National Public Health Capacities and on IHR Implementation: report by the Director‐General, March 27, 2015: para. 17. Available at http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_22Add1‐en.pdf (accessed 30 May 2020).
[17] Gostin and Katz, 2016.
[18] Suggestion from the IHR Review Committee on Second Extensions for Establishing National Public Health Capacities and on IHR (2005) Implementation. See WHO, country implementation guide 2018, available at https://apps.who.int/iris/bitstream/handle/10665/276175/WHO-WHE-CPI-2018.48-eng.pdf?sequence=1 (accessed May 2020).
[19]WHO, available at https://www.who.int/ihr/procedures/mission-reports/en/ (accessed May 2020). See also the CDC website (US), https://www.cdc.gov/globalhealth/healthprotection/stories/global-jee-process.html (accessed 30 May 2020).
